Document Type : Original Article
Authors
- Muna Mohammed Yaseen 1
- Sami Awad Alkubaisy 2
- Walid Theib Mohammad 3
- Abduladheem Turki Jalil 4
- Saja Hussain Dilfy 5, 6
1 Basic Science Department, Dentistry of College, University of Anbar, Al-Anbar, Iraq
2 Desert Studies Center, University of Anbar, Al-Anbar, Iraq
3 Al-Hussein Bin Talal University, Princess Aisha Bint Al Hussein College for Nursing and Health Sciences, Princess Aisha Nursing College, Jordan
4 Medical Laboratories Techniques Department, Al-Mustaqbal University College, Babylon, Hilla, 51001, Iraq
5 Medical Laboratories Techniques Department, the Islamic University, College of Technical Engineering, Najaf, Iraq
6 Department of Biology, College of Education for Pure Science, Wasit University, Iraq
Abstract
Diabetes is one of the health challenges for decades, which is concurrent with many pathological disorders. Hence so the aim of the current study aims is to clarify the relationship between type 2 diabetes and peptic ulcers, in addition to knowing its causes and ratio among the population of Wasit city. This study was conducted on 100 patients with type 2 diabetes aged between 20-80 years and 50 non-diabetics with a peptic ulcer as a control group. Medical and laboratory tests to identify diabetes mellitus and peptic ulcers were conducted in at Al-Zahraa General Teaching Hospital. The current study showed that most of the diabetic patients are in the age group from 60 to 80 years, and most of the patients were males (53%). The results of the present research showed that the main leading cause of type 2 diabetes are is a family genetic predisposition to diabetes (44%). Also, exposure of some individuals to a sudden psychological or nervous shock had a role in the occurrence of diabetes by 24%. In our research, 55% of the diabetic patients suffer from peptic ulcers (55/100 persons) and mainly appeared among males (29 males (53%)) compared to females (26 females (47%)). The clinical and laboratory tests showed that Helicobacter pylori (H. pylori) infections were more virulent on in the digestive system of diabetic patients compared to the than non-diabetic patients. The results showed that the occurrence of peptic ulcers in both the stomach and duodenum appeared clearly in diabetic patients, where whereas 42% of diabetic patients had simultaneous ulcers in the stomach and duodenum at the same time. The endoscopic test detected that high-risk hemorrhage Forrest IA, IB, and llA were mainly identified in diabetic patients at a percentage of 18.5%, 15%, and 13%, respectively. Patients with type 2 diabetes have a significant risk for of developing peptic ulcer hemorrhage.
Graphical Abstract
Keywords
Main Subjects
Introduction
Diabetes is a chronic disease when the pancreas fails to produce enough insulin or the body's insulin is not utilized adequately [1]. Insulin is a hormone that helps to regulate blood sugar levels. Hyperglycemia, or a high blood sugar level, is a common complication of untreated diabetes, and it can impair a range of body systems over time, especially nerves and blood vessels. Diabetes affected 8.5 percent of persons aged 18 and above in 2014. In 2012, diabetes was the direct cause of 1.5 million deaths, while high blood glucose caused 2.2 million deaths [2-4].
Diabetes mellitus is classified into two types: type 1 and type 2. Many earlier terminologies, such as juvenile diabetes or insulin-dependent diabetes, have been replaced by the phrase type 1 diabetes. Similarly, the term "type 2 diabetes" has supplanted phrases like "adult diabetes," "obesity-related diabetes," and "non-insulin-dependent diabetes". Other than these two varieties, there is no agreed-upon name for the rest of the species; for example, some sources refer to type 3 diabetes as “gestational diabetes". [5,6].
Gastrointestinal disorders are common among all people, including those with diabetes, where the chances of a digestive problem are greater, whether it is peptic ulcers, gallstones, irritable bowel syndrome, food poisoning, or other diseases [7,8]. Furthermore, reduced gastric secretion (in response to insulin but not to histamine or pentagastrin) and motility are frequently found in patients with chronic diabetes. Diabetes mellitus has been linked to a decrease in gastric acid secretion or an increase in acid output, and an increased risk of developing a peptic ulcer. Some studies have shown that diabetes affects the secretion of stomach acid and causes indigestion due to a lack of gastric juice. It also increases the chances of infection with fungal, bacterial, or amoeba infections, which may be accompanied by ulcers in the digestive system [9-11]. H. pylori is a gram-negative, microaerophilic bacteria that colonizes the human stomach mucosa. Nearly all hosts experience local inflammation after H. pylori infection. Atrophic gastritis, intestinal metaplasia, and non-cardia gastric are all linked to this ongoing process [12,13]. Although many studies have found a link between H. pylori infection and type 2 diabetes, others have found a weak or non-existent link. Studies that explain the mechanism of peptic ulcers in diabetic patients are limited, so the current study attempts to demonstrate this disorder [14].
Aim of the study
Many previous studies have focused on the gene polymorphism that controls diabetes and the role of the immune response in disease progression. According to our knowledge, there are limited studies that determine the role of diabetes in the occurrence or development of peptic ulcers. Therefore, the current study aims to:
- Determine the incidence of peptic ulcers in diabetic patients.
- Identify the effect of diabetes mellitus on the development of peptic ulcers by comparing the severity and locations of peptic ulcers in diabetic patients with non-diabetics.
- Determine the rate of type 2 diabetes in males and females.
- Determine the leading causes of diabetes in adults.
Patients and Methods
Samples
The current study is a case-control study conducted on patients with diabetes hospitalized in Al-Zahraa Teaching Hospital from January to April 2020. This study was performed by taking blood samples from 100 diabetic patients who were clinically diagnosed by specialized doctors. The study also included 50 with peptic ulcers and not suffering from diabetes as a control group. In addition, stool specimens took from diabetes and control group with symptoms of peptic ulcer. Also, all patients and individuals in the control group agreed with the (Arab) ethnicity of Al-Zahraa Teaching Hospital. Before collecting information and conducting tests, consent was obtained from all participants
Tests used for diabetes
Measuring blood sugar is one of the most common tests that are done in laboratories, and its importance is due to the early detection of diabetes cases. Most importantly, the detection of diabetic intolerance, is the condition that precedes the accidental occurrence of diabetes. The importance of measuring glucose is also due to the follow-up treatment for diabetes mellitus and to know whether the condition is stable or unstable. This study covers the following tests: Fasting blood glucose, Random blood sugar, Post Prandial Blood sugar, Oral Glucose Test, Pregnant Diabetic Test, HBA1C, and Proinsulin Test [15].
Diagnosis of peptic ulcer
In this research, blood, stool, and breathing tests were performed if the patient has peptic ulcer, or another disease (such as indigestion or irritation/irritation of the mucous layer of the stomach) whose symptoms are similar to those of peptic ulcers, in order to look for the presence of H. pylori. The blood test procedure depends on the detecting of antibodies against H. Pylori in blood using AimStep H.Pylori kit/AMAZON. (The One Step H. pylori Antigen Rapid Test is an in vitro qualitative immunochromatographic assay for rapidly detecting H. pylori antigens in human stool specimens using Pylori Antigen Rapid Test Kit/ USA). In addition, the Urea 13C Breath Test kit is based on the secretion of much active urease by gastric H. pylori that can break down urea into ammonia and carbon dioxide (CO2).
Endoscopic test
Esophagogastroduodenoscopy procedure is performed by passing a flexible endoscope through the mouth into the esophagus, stomach, and duodenum. This is the best approach for inspecting the gastrointestinal mucosa and may be conducted under conscious sedation in most patients. It has been used to determine the location, size, and shape of peptic ulcers and whether or not the ulcer is accompanied by bleeding.
Classification of peptic ulcer
According to endoscopic test, the clarification of stigmata of recent hemorrhage of peptic ulcer are performed as following Table 1;
Table 1: Classification of peptic ulcer depending on the endoscopic test
|
Sitgmata of hemorrhage |
Forrest classification [18] |
|
Active spurting bleeding |
IA |
|
Active oozing bleeding |
IB |
|
Non-bleeding visible vessel |
IIA |
|
Adherent clot |
IIB |
|
Flat pigmented spot |
IIC |
|
Clean base |
III |
Statistical Analysis
The current data were analyzed using Excel 2010 and the Statistical Package for Social Sciences (SPSS 19) program and social sciences system, with results considered statistically significant if the P value was less than 0.05.
Results
The current study included 100 diabetic patients diagnosed laboratory and clinically in Al-Zahraa Teaching Hospital. Their ages ranged from 20 to 80 years, with an average age of 50.82 ± 9.21 years, as shown in Table 2, and most of the patients were males (53%) while the number of females was 47 (47%), as in Figure (1). On the other hand, the distribution of patients according to gender or age groups did not show clear statistical differences (p<0.05). The current study also showed that most (40 individuals) diabetic patients are in the age group of 60 to 80 years as in Table 3.
The control group included 50 individuals suffering from peptic ulcers and non-diabetics; their ages ranged from 19 to 79 years, with an average age of 48.39 ± 7.88. Furthermore, significant differences in the age mean did not appear when comparing the group of patients with the control (P= 0.252), as shown in table 2.
Table 2: Comparison age mean of patients and controls
|
Age/year |
Cases |
Control |
P value |
|
Age range |
20-80 |
19-79 |
0.252 |
|
Mean± SD |
50.82±9.21 |
48.39±7.88 |
|
|
SE |
0.941 |
0.788 |
|
|
Total number |
100 |
50 |
SD= Standard Deviation; SE= Standard Error

Figure 1: Distribution of diabetic patients depending to on gender
Table 3: Gender and age groups of diabetic patients
|
Case number |
Age range |
Age mean ± SD |
Females |
Males |
P value |
|
27 |
20-40 |
26.8+3.88 |
11(41) |
16(59) |
0.056 |
|
33 |
40-60 |
47.78+9.41 |
18(55) |
15(45) |
0.053 |
|
40 |
60-80 |
67.28+10.1 |
18(45) |
22(55) |
0.054 |
SD= Standard Deviation
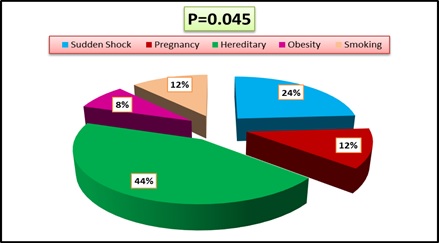
The results of the current research showed that 44% of diabetic patients were the causes of their disease as a result of their family genetic predisposition to diabetes; furthermore, the exposure of some people to a sudden psychological or nervous shock had a role in the occurrence of diabetes by 24%, while pregnancy was the cause of diabetes in women at rate 12%, so smoking had the same percentage in the incidence of diabetes, in addition, the role of obesity in the occurrence of diabetes was detected in 8% of patients as in Figure 2.

Figure 2: The causes of diabetes mellitus
More than half (55%) of the diabetic patients in the current study suffer from peptic ulcers (55/100 persons), where ulcers were more clearly identified in males (29 males (53%)) compared to females (26 females (47%)) however there are not significant differences (P= 0.101) in the incidence of ulcerative diabetes according to the gender as in Figure 3.
The clinical and laboratory tests showed that H. Pylori infection was more virulent in diabetic patients’ digestive systems than in non-diabetic ones. The results showed that peptic ulcers in both the stomach and duodenum appeared clearly in diabetic patients, whereas 42% of diabetic patients had simultaneous ulcers in the stomach and duodenum. In comparison, those ulcers appeared in 16% of the non-diabetic patients, leading to statistical emergence (p=0.003). On the other hand, ulcers in one tissue (stomach or duodenum) mainly appeared in people without diabetes, as shown in Table 4.

Figure 3: Percentage of peptic ulcer among diabetic patients
Table 4: Prevalence peptic ulcer according to site of the H. Pylori infection
|
Site of ulcers |
Cases |
Control |
P value |
|
N (%) |
N (%) |
||
|
Stomach and duodenum |
23 (42) |
8 (16) |
0.003* |
|
Stomach |
15 (27) |
24 (48) |
0.016* |
|
Duodenum |
17 (31) |
18 (36) |
0.277 |
*Significant (p < 0.05); N= Number
The prevalence of ulcers with stigmata of recent bleeding represents the severity of peptic ulcers from infection by H. pylori (Table 5). Index of endoscopic test detected high-risk hemorrhage Forrest IA, IB and llA generally detected in diabetic patients at percentage; 18.5%, 15%, and 13% respectively. Adherent clots (grade IIB) primarily developed in non-diabetic patients (26%) and were red, maroon, or black with an amorphous texture that could not be removed by suction or strong water irrigation. Flat, pigmented spots (grade IIC) and clean-base ulcers (grade III) are other low-risk lesions mostly found in non-diabetic people at 40% and 20%, respectively.
Table 5: Prevalence of peptic ulcer severity according to Forrest classification
|
Forrest classification |
Cases (N=54) |
Control (N=50) |
P value |
|
IA |
10(18.5) |
2 (4) |
0.043* |
|
IB |
8 (15) |
0 (0) |
0.011* |
|
IIA |
7 (13) |
5 (10) |
0.360 |
|
IIB |
9 (17) |
13 (26) |
0.051 |
|
IIC |
17 (31) |
20 (40) |
0.053 |
|
III |
3 (5.5) |
10 (20) |
0.025* |
*Significant (p < 0.05); N= Number
Discussion
Type 2 diabetes occurs due to the ineffectiveness of the body's ability to use insulin. Most of the time, it occurs due to being overweight and physical inactivity, represented by lack of movement. Its symptoms are similar to type 1 but may be less pronounced in many cases, so the patient may be diagnosed several years after the symptoms began [16,17]. When the patient reaches the age of 20 years, that is, after complications occur, which was shown in the current study, but there are studies confirming the emergence of this pattern in childhood [18]. This study also agrees with what Garagnani and his colleagues mentioned in 2013, that the risk of developing type 2 diabetes increases with age, especially after the age of 45 years, because after this age, movement and exercise decrease, and this leads to a lack of muscle in the body and weight gain, while other studies have shown that diabetes spreads between the ages of 30 and 40 years due to lack of activity and overweight [19,20]. The current study also showed that the incidence of diabetes in men is more than in women, perhaps due to the influence of male hormones, smoking, and lack of movement in men compared to women [21].
According to current research, Type 2 diabetes is caused by a confluence of lifestyle and genetic factors; while certain aspects, such as nutrition and obesity, are under control, others, such as age, gender, and genetic factors, are not [22]. Most cases of diabetes in current the study have a positive family history of diabetes mellitus, which confirms the role of genetic genes in the occurrence of the disease in some people [23]. A study in 2011 identified that more than 36 genes had contributed to type 2 diabetes. Together, these genes make up only 10% of the total inherited components of the disease [24,36-37]. For example, the TCF7L2 allele increases the risk of diabetes by one and a half times. The greatest risk comes from shared genetic variants, and most of these genes associated with diabetes are involved in beta cell functions [25]. Moreover, sudden shock appeared as the second cause of diabetes mellitus in our study, which may be related to nerves and gland dysfunction. The adrenal glands increase in size and secrete two hormones (adrenaline and noradrenaline) when the body is exposed to a sudden nervous or psychological shock or stress [22]. Adrenaline is an essential substance for regulating the level of glucose in the blood. Raising blood sugar is essential in stressful situations, as the body prepares itself for physical and mental activity [36,37]. The secretion of adrenaline helps achieve this, and it also ensures that, in addition to increasing blood pressure, oxygen and glucose provide to all body parts. For those who do not suffer from diabetes, the body secretes insulin to reduce high blood sugar, while in the case of diabetes, stress may contribute to an increase in blood sugar for several days, weeks, or months [11].
The current study shows that pregnancy leads to diabetes in some women, and this may be due to weight gain and poor glucose levels during pregnancy as a result of hormonal changes, in addition to the placenta secretion of hormones that stop the performance of the hormone insulin in the blood during pregnancy, thus increasing the level of sugar [13]. On the other hand, some medical research has documented that the increase in the proportion of fluid around the fetus in the womb of a pregnant woman may be one of the factors that cause diabetes [22].
Smoking and diabetes mainly target the body’s immunity, as they affect one way or another negatively on the body’s functions. Over the years, many studies and research have been conducted that confirmed the existence of a strong link and relationship between smoking and type 2 diabetes. Smoking helps to raise the blood sugar level to a high level compared to normal people [23]. The high number of cigarettes smoked daily increases the risk of developing type 2 diabetes. This is due to the nicotine in tobacco, which has an essential role in weakening insulin sensitivity [24].
The current clinical and laboratory tests showed that H. Pylori infection was more virulent in the digestive system of diabetic patients than the non-diabetic people, so 42% of diabetic patients had ulcers in the stomach and duodenum at the same time. Moreover, the index of endoscopic test detected that high-risk hemorrhage Forrest I and llA in 25/55 diabetic patients while it appeared in 7/50 non-diabetic patients. Previous research has indicated that diabetic patients may have poorer outcomes after peptic ulcer complications caused by diabetic angiopathy, blurring of symptoms caused by autonomic neuropathy, delayed ulcer healing, and an increased risk of bacterial sepsis [20]. Due to the considerable sample size required to explore this topic, there is relatively little data on the relationship between diabetes and outcome after peptic ulcer complications [18]. Our findings back with a prior study that indicated diabetes people have a higher rate of peptic ulcer illness than the general population. Furthermore, in animal investigations, diabetic rats show delayed gastric ulcer healing and increased stomach mucosal sensitivity to ulcer-causing or stress-inducing medications [17].
Diabetes-related gastric mucosa lesions have previously been documented to include desquamation of the surface epithelium with diffuse hemorrhage and severe hemorrhage with localized erosion [1]. The deformation of the normal morphology of parietal cells in diabetes patients may contribute to the low level of stomach acid output. Diabetes causes cellular and functional alterations in the glandular stomach, particularly in the parietal cells, such as a decrease in the number of mitochondria accompanied by a drop in H+-K+-ATPase and canaliculi [6]. In diabetic patients, however, micrographs of the stomach mucosa demonstrate that parietal cells are unevenly spread, and some necrosis areas develop compared to normal mice. Furthermore, normal epithelial cells are well-defined, whereas diabetic mice's epithelial cells are fragmented and more widespread [8,9]. This is consistent with earlier studies that diabetes has a negative impact on the gastrointestinal tract [11,12]. However, our findings contradict a study that found no significant difference in H. pylori infection between those with and without diabetes who had a peptic ulcer/erosion [15].
Additionally, a link has been established between H. pylori seropositivity, H. pylori cagA positivity, and higher mean HbA1c values, a marker of chronic diabetes. Furthermore, another study involving Taiwanese patients found that chronic H. pylori infection raises HbA1c levels while lowering insulin synthesis [20]. On the other hand, some research revealed no relationship between H. pylori and diabetes. Xia et al. discovered no significant difference in H. pylori seropositivity between diabetes and non-diabetic subjects in their investigation [23,26-28]. Oluyemi et al. in Nigeria and research from Romania, Italy, China, and Turkey [18.12] found comparable results [56,57,58,59]. The genetic diversity of H. pylori strains could explain the discrepancies in data about the relationship between H. pylori and diabetes. Significant geographic genetic diversity in particular virulence genes (cytotoxin-associated gene product (CagA), the vacuolating toxin (VacA), and the adhesion protein (BabA2) has been discovered, which contributes to the varying risk of H. Pylori infection's mixed clinical results [25,29-35].
Conclusion
The conclusion from the current study is that 55% of patients with type 2 diabetes suffer from peptic ulcers resulting from H. pylori infection, as 42% of those suffering from ulcers in the stomach and duodenum, while it appeared in 4% of non-diabetics, on the other hand, peptic ulcers were more severe and accompanied by bleeding in a good group of diabetic patients, while it was rare in non-diabetic individuals.
Recommendations
The effect of diabetes on the occurrence of ulcers in the duodenum is not clear, so it is preferable to conduct a later histopathological study that includes a larger number of diabetic patients with duodenal ulcers, in addition to conducting studies to obtain a new treatment that supports the tissues of the digestive system and reduces the effect of abnormal insulin levels on the development of peptic ulcer and other digestive disorders.
Ethical approval
All procedures performed in studies involving human participants were in accordance with under the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
This research did not receive any specific grant from fundig agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed to data analysis, drafting, and revising of the paper and agreed to be responsible for all the aspects of this work.
Conflict of Interest
The author declared that they have no conflict of interest.
ORCID:
Muna Mohammed Yaseen
https://orcid.org/0000-0002-1438-5680
Sami Awad Alkubaisy
https://orcid.org/0000-0002-9565-8395
Walid Theib Mohammad
https://orcid.org/0000-0002-2687-0552
Abduladheem Turki Jalil
https://orcid.org/0000-0001-8403-7465
Saja Hussain Dilfy
https://orcid.org/0000-0002-2274-7960
HOW TO CITE THIS ARTICLE
Muna Mohammed Yaseen, Sami Awad Alkubaisy, Walid Theib Mohammad, Abduladheem Turki Jalil, Saja Hussain Dilfy. Cancer and Complications of Peptic Ulcer in Type 2 Diabetes Mellitus patients at Wasit province, Iraq. J. Med. Chem. Sci., 2023, 6(2) 335-345