Document Type : Original Article
Authors
1 Faculty of Biology and Ecology, Yanka Kupala State University of Grodno, 230023 Grodno, Belarus
2 Medical Laboratories Techniques Department, Al-Mustaqbal University College, Babylon, Hilla, 51001, Iraq
3 Al-Hussein Bin Talal University, Princess Aisha Bint Al Hussein College for Nursing and Health Sciences, Princess Aisha Nursing College, Jordan
4 Dean Faculty of Biology and Ecology, Yanka Kupala State University of Grodno, 230023 Grodno, Belarus
5 Medical Laboratories Techniques Department, the Islamic University, College of Technical Engineering, Najaf, Iraq
6 Department of Biology, College of Education for Pure Science, Wasit University, Iraq
Abstract
Cervical cancer is the third most prevalent form of cancer among all types of cancer in the developing world. Adequate and improved screening programs for the detection of cervical cancer and a better understanding of its association with human papillomavirus (HPV) have decreased disease cases in developed countries. The study’s goal conducted is early detection of cervical lesions that can potentially transform into cervical cancer. Observed data demonstrate a differential prevalence of cervical cancer in women from different age groups. 37% of women affected are in the age group 43-52 years, followed by 30% of women aged 32-42 and 20% aged 63-78. Different pathological changes observed with cervical cancer include squamous cell carcinoma in the cervix, keratinization of squamous cells, nuclear polymorphism, and necrosis, with 40% and 32% of cancer cases reaching invasive stages III and IV, respectively. Only 5% of cases detected are in the noninvasive stage, stage 0, and 11% in stage II. Results from the current study also demonstrates the differential distribution of cancer stages concerning different age groups. Stage III cancer was predominantly observed in patients from the age group I, II, and III (42%, 41%, and 39%, respectively). In contrast, increased metastatic cancer or stage IV was mostly observed in women from age group IV (47%) comprising older patients. The current study also showed increased cases of cervical cancer affecting women from the Dhi- Qar governorate and its risks proportional to the age of women. Lack of access to a proper clinical test and widespread infection of HPV added to lack of vaccination, and proper treatment further enhances the cancer cases amongst the women from Dhi Qar governorate.
Graphical Abstract
Keywords
Introduction
Cervical cancer is one of the most common cancers affecting women’s health and is ranked the third most common cancer affecting the female population. More than a million women worldwide are currently affected by cervical cancer, with most undiagnosed cases. Lack of access to proper treatment for cure and prevention contributes to cancer-related deaths [1, 2].
Low to middle-income countries display significantly increased numbers of cervical cancer-related deaths. In 2012, 528 000 women were diagnosed with cervical cancer, and 266000 women were reported dead, of which 90% were reported to be from low to middle-income countries. The mortality rate is estimated to increase by almost 25% in the next ten years due to cervical cancer [2, 3].
Over the past 50 years, the population’s access to preventative measures has displayed a 50-70% decrease in cervical cancer-related mortality. American Cancer Association guidelines suggest vagina and cervix smear, pap test, and the HPV DNA test as a diagnostic test for cervical cancer in asymptomatic women. It can also be used as a diagnostic method for women undergoing pre-invasive cervical cancer treatment [4, 5]. Previous studies on high-risk human papillomavirus (hr-HPV) and its association with cervical cancer have resulted in the development of biomolecular tests for screening preneoplastic cervical lesions [6, 7].
HPV vaccinations produced for cervical cancer prevention pose cost issues and do not eliminate the necessity for screening. Cervical cancer is frequently related to AIDS because HIV frequently coexists with HPV. The diagnostic screening procedures utilized are equally effective and trustworthy for HIV-positive and HIV-negative women. The research’s purpose is to discover cervical lesions that have the potential to develop into cervical cancer as early as possible, and screening programs intend to lower the prevalence of cervical cancer and, consequently, the mortality linked with it.
Material and Methods
Study design
The present study was conducted in Dhi-Qar province of Iraq at the Histopathological facility of Al- Hussein Teaching Hospital and the Yanka Kupala State University of Grodno between 2017 and 2020. This study was conducted under the ethics of Al-Hussein Teaching Hospital, and consent documents were obtained from all the patients and hospital administration. Verbal consent was also obtained from the participants of the study.
Sample Collection
Sixty healthy women were selected for the control group, and samples were collected. Ninety-three samples of cervical cancer tissues were taken from the samples stored at the hospital from 2017 to 2020. Each sample collected was labeled and segregated as per year of collection, name, and age of the patient. All the samples were histologically diagnosed and segregated according to cancer diagnosed stage.
Histopathological Study
Detailed histopathological study of 93 cervical cancer tissue samples and 60 curettage samples as the control samples were conducted at Al- Hussein Teaching Hospital in the histopathological unit in Dhi-Qar Governorate, Iraq. The protocol followed for the study was as described by [12]. The tissue samples were first fixed using formalin solution, followed by tap water rinsing for 2-3 hours to remove the leftover formalin solution. The samples were subjected to dehydration, clearing, infiltration, embedding, sectioning, and staining.
Statistical analysis
Statistical Package for Social Sciences version 20 (SSPS20) and Microsoft Excel 2010 were used, and data having a P-value < 0.05 was considered statistically significant.
Results
The present survey was conducted on tissue samples obtained from 93 women suffering from cervical cancer and 60 healthy females as the control group from 2017 to 2020. The patients diagnosed with cancer ranged from 32-78 years old. The mean age of patients observed was 49.34±3.94 years compared to 45.71±4.61 mean age of the control group amongst 60 women in the age range of 32-77 years. Characteristics of the studied subjects’ different age groups of the patient are depicted in table 1. The observed data shows 37% of women aged between 43-52 years suffering from cervical cancer, 30% in the age group of 32-42 years, and 20% in the age group 63-78 years. A significant difference (p=0.0438) was observed among different groups.
Table 1: Age comparison of patients and healthy control group
|
Case-control comparison |
|||
|
Ages / years |
Patients group |
Healthy control group |
P-value |
|
Age range |
32-78 |
32-79 |
|
|
Mean ±SD |
49.34±3.94 |
45.71±4.61 |
0.432 (NS) |
|
SE |
0.51 |
0.60 |
|
|
Age groups |
N (%) |
N (%) |
|
|
Group 1 (32-42) |
28 (30) |
17(28) |
0.877(NS) |
|
Group 2 (43-52) |
34 (37) |
19(32) |
0.473(NS) |
|
Group 3 (53-62) |
12 (13) |
9(15) |
0.877(NS) |
|
Group 4 (63-78) |
19 (20) |
15(25) |
0.371(NS) |
|
N |
93 |
60 |
|
NS= No Significant (p > 0.05); SD= Standard Deviation; SE= Standard Error; N= Number
Histological examination was performed on all the histological laboratory samples to determine the cancer stage for tissue samples (figure 1, 2, 3, 4, 5, 6, 7). Different pathological changes were observed in samples, including high to low differentiated cervical squamous cell carcinoma, nuclear pleomorphism, keratinization, and necrosis. Figure 7 describes the stages of cervical cancer according to the International Federation of Gynecology and Obstetrics (FIGO) [10]. The result of the study shows a maximum number of cases in invasive stages of cancer, 40% cases in stage III and 32% in stage IV, and only 5% and 11% of the cases were observed to be in stages 0 and II, respectively.
The result of the study conducted displays differential prevalence of cancer stages concerning the age of the individuals, as depicted in figure 8. Stage III cancer was most prevalent in age groups 1, 2, and 3, of which 42% of patients belonged to group 1, 41% to group 2, and 39% to group 3. In contrast, the elderly patients displayed cancer in more metastatic phase or stage IV (47%).

Figure 1: Normal cervical squamous epithelium (black arrow), nucleus (red arrow), and cytoplasmic (yellow arrow) (40X)

Figure 2: Squamous epithelium (black arrow) with mild mixed inflammation and transformation zone (yellow arrow) (10x)

Figure 3: Poorly differentiated cervical squamous cell carcinoma: shows marked nuclear pleomorphism (green arrow) with minimal keratinization and necrosis (yellow arrow) (40x)

Figure 4: moderately differentiated cervical squamous cell carcinoma: shows keratinization (yellow arrow) and minimal nuclear pleomorphism (green arrow) (40x)

Figure 5: well-differentiated cervical squamous cell carcinoma: shows marked keratinization (yellow arrow) and minimal nuclear pleomorphism (green arrow) (10X)

Figure 6: well-differentiated cervical squamous cell carcinoma: shows marked keratinization (green arrow) and nuclear pleomorphism (yellow arrow) (40x)
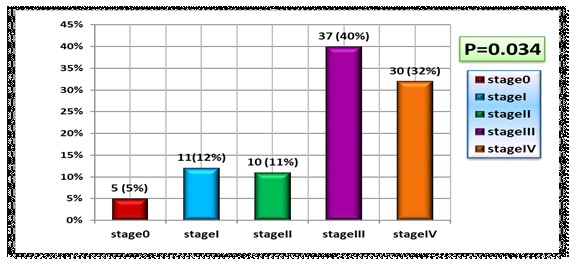
Figure 7: Distribution of cases according to cervical cancer stages (P=0.034)
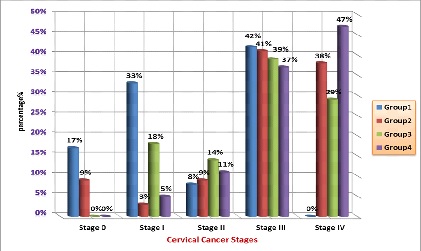
Figure 8: Distribution of the cancer stages according to age groups
Discussion
Cervical cancer affects women from of wide broad age demographics, but the increased incidences of young women suffering from cervical cancer have led to an emphasis on emphasized its study [8]. HPV is one of the major primary reasons causing cervical cancer. Lack of knowledge in younger women about sexually transmitted diseases with multiple sexual relationships drives the exponential curve for the disease. The results of the study show cervical cancer to study results show cervical cancer is more common in women under the age range of 32-25 years old. It is deduced that elevated cases of HPV infections could be driving the observed-increased cancer rates among young women. Other studies conducted have reported 38% cervical cancer rates between 2009-2013, primarily in women 55 years of age or over, and 20% of cases were reported from women aged over 65. The data from such studies hold value due to an increase in the elderly population in the coming years [9,10].
Data from Japan was observed to follow the same trend, women in the age group between 30-40 were extremely highly susceptible to the disease when compared to women from the age group 50-60, and a further spike in cancer cases was observed for women over the age of 70 [11, 12]. Sarma et al. (2021) describe the cervical cancer’s bimodal age distribution pattern for cervical cancer with two peaks between 30 to 39 years and 60 to 69 years [13]. Data observed from hospital-based cancer registries (HBCR) of India report that the mean age of cervical cancer cases registered is in the age range of 50-56.7 years, with 15% of registered cases of patients above the age of 65 years. With an increase in life expectancy, an increased incidence of cervical cancer is observed in elder women [14, 15].
The current study uses a histological examination of the cancer tissues to understand the prevalence of cancer. Past studies have reported multiple clinical presentations associated with carcinoma of the cervix. Papanicolaou (Pap) smear is one of the routinely used tests a routinely used test for cancer diagnosis in asymptomatic patients. The patients may display a varied range of symptoms which includes various symptoms, including irregularity in vaginal bleeding or metastatic cancer mass lesions, which can also be observed during the late phase of cancer [16, 17]. Cervix diagnosed with early stages of cancer often displays an eroded appearance prone to bleeding on contact; however, nodular, ulcerated lesions, or an exophytic mass are characteristics of more advanced stages of cancer. Other symptoms include an endophytic growth in the cervical canal which gets infiltrated into the wall resulting in the hardening of the cervix. Due to which this, the malignant cells present in the underlying tissue might escape detection using a cytological smear. Cervical cancer is of many types; few cervical cancers grow endophytically from the cervix canal without causing gross abnormality [18]. An increased cervix with a bulkier appearance larger than 6cm in size is called the barrel-shaped cervix. such These observations are associated with different types of tumors, but it is more commonly seen in adenocarcinoma [19,20].
Previous research has reported the extension of cervical cancer predictably, and it locally involves extension into the endometrium more than an upper vagina. Lymph-vascular space invasion also causes parametrial involvement. The tumor can proceed laterally, anteriorly, or posteriorly from the parametrium; it can extend to the pelvic sidewall, bladder base, or rectum respectively. The local spread of cancer to the endometrium and fallopian tubes can also be observed in a few cases [21, 22]. The International Federation of Gynecologists and Obstetricians (FIGO) upgraded its system for classifying the clinical stages of cancer in 2009; various issues considered for the updated system include surgical vs. clinical staging, the addition of further substages, and early invasion, among others [23, 24]. The cervical squamous cells cancer cells are graded according to the degree of keratinization, cytological atypia, and mitotic activity, with the invasion pattern observed for cancer also being a parameter.
The cancer cells have classification and subclassifications based on large cell keratinizing, large cell non-keratinizing, and small cell non-keratinizing categories regarded as well, moderately and poorly differentiated cancers, respectively [25]. However, conflicting reports suggest a poor prognosis of keratinizing variants in comparison compared to non-keratinizing variants of squamous cells. Previous studies conducted have reported that differentiated keratinizing cancer cells in the vulva for non-HPV-related cancers display a poor prognosis in comparison compared to differentiated HPV-related non-keratinizing neoplasms [20]. The World Health Organization (WHO) suggests the grading system for cervical squamous cells carcinomas based on various parameters, including the degree of keratinization, nuclear pleomorphism, size of nucleoli, mitotic frequency, and necrosis, but the detailed application of the parameters to grade the carcinomas has not been provided [22].
Stendahl et al. report the usage of using a multifactor grading system involving the tumor and stromal parameters. A total of 8 features were assessed for the grading of cancer cells and included parameters such as (growth pattern, differentiation, pleomorphism, mitoses, pattern of invasion, depth of invasion, lymphovascular space invasion, and inflammatory reaction) [23]. Further modification adopted by Stendahl et al. uses patterns of tumor invasion as a grading system. This multifactor system considered the depth of invasion and lymphovascular space invasion for grading cancer cells; such factors were not traditionally used for grading squamous cells and were reported in the pathology report [20].
Histological screening of cervical cancer has immense potential for proper prognosis and helps reduce metastatic cancer cases and mortality associated with it [19]. Recent data show reduced incidence of squamous cell carcinoma attributed to proper screening of cervical cancer but may not have any significant impact on significantly impact adenocarcinoma of the cervix [15, 16]. Women participating actively in screening programs are diagnosed at early stages of cancer [16]. Hence it was concluded that population-based screening programs in many countries assist in screening patients and enable extended survival of women displaying metastatic stages of cancer [12]. Results of the study showed increased incidences of patients in metastatic stages of cancer, namely cancer stage III (40%) and IV (32%), and also reports differential age distribution of patients in association to cancer stage as depicted in figure 8. Stage III cancer is observed in women between age groups 32-42 years (42%), 43-52 years (41%), 53-62 years (39%), whereas 47% of older patients from age group 63-78 years display a more aggressive metastatic stage IV of cancer.
The variation observed among different age groups could be a predisposition of genetic factors associated with patients or environmental factors such as exposure to radioactive or toxic materials. Increased HPV infections are also responsible for the data observed and will be discussed later in this chapter [5]. Pelkofski et al. reported small cell carcinoma in 2% of patients, a mean incidence of 0.06 per 100,000 women has been observed with this aggressive histology, and this might affect our findings [10,11]. Castanon et al. examined 1800 women aged 20-29 between 2007-2012 with cervical cancer and observed 2% low non-squamous, non-adenocarcinoma, and non-adenosquamous. This observed histological subtype was mostly observed at 6% in very young women between 20-24 years; this subset of women has been chiefly diagnosed with stage II cancer in comparison to women at 25 years of age of between 26-29 years with 4% and 7% frequency respectively. The result of the study was in accordance with a study conducted by Pelkofski et al., where 17% of the patients aged between 20-29 years were diagnosed with stage II cervical cancer [12,13].
The present result observed is in accordance with the study conducted by Dutta et al. (2013) reported that 85% of patients in the late stages of cancer and 63-89% of patients display cancer properties associated with stages I and II [8]. There are conflicting reports on the relationship between age at diagnosis and prognosis. Rutledge et al. studied 250 women aged below 35 years alongside older women and reported decreased overall survival of younger women who were diagnosed with advanced stages of cancer but survived longer upon early diagnosis [18]. Studied and compared 41 women aged 35 with 96 women aged less than 36 and observed intense aggression of cervical cancer and increased nodal metastases in younger patients with initial stages of cancer in comparison with older women [25].
Conclusion and Recommendation
The study concludes that increased mortality rates and higher cases of metastatic cervical cancer are attributed to a lack of histological examinations and vaccines against HPV. The present study also recommends further investigation of the relationship between hr-HPV stages and stages of cervical cancer. The results observed indicate the prevalence of cervical cancer in Dhi Qar Governorate; hence various healthcare programs can be introduced in the region for the welfare of the women.
Ethical approval
All procedures performed in studies involving human participants were under the ethical standards of the institutional or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
This research did not receive any specific grant from fundig agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed to data analysis, drafting, and revising of the paper and agreed to be responsible for all the aspects of this work.
Conflict of Interest
The author declared that they have no conflict of interest.
ORCID:
Abduladheem Turki Jalil
https://orcid.org/0000-0001-8403-7465
Walid Theib Mohammad
https://orcid.org/0000-0002-2687-0552
Aleksandr Karevskiy
https://orcid.org/0000-0003-1340-1551
Saja Hussain Dilfy
https://orcid.org/0000-0002-2274-7960
HOW TO CITE THIS ARTICLE
Abduladheem Turki Jalil, Walid Theib Mohammad, Aleksandr Karevskiy, Saja Hussain Dilfy. Histological Diagnosis and Staging of Cervical Cancer Samples Collected from Women in Dhi-Qar Province. J. Med. Chem. Sci., 2023, 6(2) 269-279
- WHO Guidelines for Screening and Treatment of Precancerous Lesions for Cervical Cancer Prevention. Geneva: World Health Organization, 2013 [Publisher]
- Comprehensive Cervical Cancer Control: A Guide to Essential Practice. 2nd ed. Geneva: World Health Organization, 2014 [Publisher]
- Turki Jalil A., Hussain Dilfy S., Oudah Meza S., Aravindhan S., M Kadhim M., M Aljeboree A., CuO/ZrO2 nanocomposites: facile synthesis, characterization and photocatalytic degradation of tetracycline antibiotic, Journal of Nanostructures, 2021, 11:333 [Crossref], [Google Scholar], [Publisher]
- Elveny M., Jalil A.T., Davarpanah A., Alfakeer M., Bahajjaj A.A., Ouladsmane M., CFD-based simulation to reduce greenhouse gas emissions from industrial plants, International Journal of Chemical Reactor Engineering, 2021, 19:1179 [Crossref], [Google Scholar], [Publisher]
- Marofi F., Rahman H.S., Al-Obaidi Z.M.J., Jalil A.T., Abdelbasset W.K., Suksatan W., Dorofeev A.E., Shomali N., Chartrand M.S., Pathak Y., Hassanzadeh A., Baradaran B., Ahmadi M., Saeedi H., Tahmasebi S., Jarahian M., Novel CAR T therapy is a ray of hope in the treatment of seriously ill AML patients, Stem Cell Research & Therapy, 2021, 12:465 [Crossref], [Google Scholar], [Publisher]
- Jalil A.T., Shanshool M.T., Dilfy S.H., Saleh M.M., Suleiman A.A., Hematological and serological parameters for detection of COVID-19, Journal of microbiology, biotechnology and food sciences, 2022, 11:e4229 [Crossref], [Google Scholar], [Publisher]
- Vakili-Samiani S., Jalil A.T., Abdelbasset W.K., Yumashev A.V., Karpisheh V., Jalali P., Adibfar S., Ahmadi M., Hosseinpour FeiziA., Jadidi-Niaragh F., Targeting Wee1 kinase as a therapeutic approach in Hematological Malignancies, DNA repair, 2021, 107:103203 [Crossref], [Google Scholar], [Publisher]
- Ngafwan N., Rasyid H., Abood E.S., Abdelbasset W.K., Al-Shawi S.G., Bokov D., Jalil A.T., Study on novel fluorescent carbon nanomaterials in food analysis, Food Science and Technology, 2021, 42 [Crossref], [Google Scholar], [Publisher]
- Marofi F., Abdul‐Rasheed O.F., Rahman H.S., Budi H.S., Jalil A.T., Yumashev A.V., Hassanzadeh A., Yazdanifar M., Motavalli R., Chartrand M.S., Ahmadi M., Cid-Arreguid A., Jarahian M., CAR‐NK cell in cancer immunotherapy; A promising frontier, Cancer Science, 2021, 112:3427 [Crossref], [Google Scholar], [Publisher]
- Jumintono J., Alkubaisy S., Singh K., Mikolaychik I., Morozova L., Effect of cystamine on sperm and antioxidant parameters of ram semen stored at 4°C for 50 hours, Archives of Razi Institute, 2021, 76:115 [Crossref], [Google Scholar], [Publisher]
- Raya I., Chupradit S., Kadhim M.M., Mahmoud M.Z., Jalil A.T., Surendar A., Ghafel S.T., Mustafa Y.F., Bochvar A.N., Role of compositional changes on thermal, magnetic, and mechanical properties of Fe-PC-based amorphous alloys, Chinese Physics B, 2022, 31:016401 [Crossref], [Google Scholar], [Publisher]
- Chupradit S., Jalil A.T., Enina Y., Neganov D.A., Alhassan M.S., Aravindhan S., Davarpanah A., Use of organic and copper-based nanoparticles on the turbulator installment in a shell tube heat exchanger: a CFD-based simulation approach by using nanofluids, Journal of Nanomaterials, 2021, 2021:3250058 [Crossref], [Google Scholar], [Publisher]
- Pecorelli S., Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium, International Journal of Gynecology & Obstetrics, 2009, 105:103 [Crossref], [Google Scholar], [Publisher]
- Goodheart M., Jacobson G., Smith B.J., Zhou L., Chemoradiation for invasive cervical cancer in elderly patients: outcomes and morbidity, International Journal of Gynecologic Cancer, 2008, 18:95 [Crossref], [Google Scholar], [Publisher]
- Otaghi M., Bastami M., Borji M., Tayebi A., Azami M., The effect of continuous care model on the sleep quality of hemodialysis patients. Nephro-urology Monthly, 2016, 8 [Crossref], [Google Scholar], [Publisher]
- Mehrpour S., Najafi A., Ahmadi A., Zarei T., Pleqi V., Basiri K., Komlakh K., Abdollahi H., Emami K.H., Relationship of the optic nerve sheath diameter and repeated invasive intracranial pressure measures in traumatic brain injury patients; a diagnostic accuracy study. Frontiers in Emergency Medicine, 2022, 6:e6 [Crossref], [Google Scholar], [Publisher]
- Shimamoto K., Saito T., Kitade S., Tomita Y., Nagayama R., Yamaguchi S., Ariyoshi K., Okadome M., A study of treatments and outcomes in elderly women with cervical cancer, European Journal of Obstetrics & Gynecology and Reproductive Biology, 2018, 228:174 [Crossref], [Google Scholar], [Publisher]
- Kunos C., Tian C., Waggoner S., Rose P.G., Lanciano R., Retrospective analysis of concomitant Cisplatin during radiation in patients aged 55 years or older for treatment of advanced cervical cancer: a gynecologic oncology group study, International Journal of Gynecologic Cancer, 2009, 19:1258 [Crossref], [Google Scholar], [Publisher]
- Yanazume Y., Yanazume S., Iio K., Yonekura R., Kojima N., Uchida N., Koriyama C., Douchi T., Major causes of impractical brachytherapy in elderly patients with uterine cervical cancer, Journal of Obstetrics and Gynaecology Research, 2014, 40:1725 [Crossref], [Google Scholar], [Publisher]
- Darvishi A., Otaghi M., Mami S., The effectiveness of spiritual therapy on spiritual well-being, self-esteem and self-efficacy in patients on hemodialysis. Journal of Religion and Health, 2020, 59:277 [Crossref], [Google Scholar], [Publisher]
- Herfs M., Yamamoto Y., Laury A., Wang X., Nucci M.R., McLaughlin-Drubin M.E., Münger K., Feldmen S., McKeon F.D., Xian W., Crum C.P., A discrete population of squamocolumnar junction cells implicated in the pathogenesis of cervical cancer, Proceedings of the National Academy of Sciences, 2012, 109:10516 [Crossref], [Google Scholar], [Publisher]
- Jumintono J., Alkubaisy S., Singh K., Mikolaychik I., Morozova L., Effect of cystamine on sperm and antioxidant parameters of ram semen stored at 4°C for 50 hours, Archives of Razi Institute, 2021, 76:115 [Crossref], [Google Scholar], [Publisher]
- Raya I., Chupradit S., Kadhim M.M., Mahmoud M.Z., Jalil A.T., Surendar A., Ghafel S.T., Mustafa Y.F., Bochvar A.N., Role of compositional changes on thermal, magnetic, and mechanical properties of Fe-PC-based amorphous alloys, Chinese Physics B, 2022, 31:016401 [Crossref], [Google Scholar], [Publisher]
- Chupradit S., Jalil A.T., Enina Y., Neganov D.A., Alhassan M.S., Aravindhan S., Davarpanah A., Use of organic and copper-based nanoparticles on the turbulator installment in a shell tube heat exchanger: a CFD-based simulation approach by using nanofluids, Journal of Nanomaterials, 2021, 2021:3250058 [Crossref], [Google Scholar], [Publisher]
- Jalil A.T., Ashfaq S., Bokov D.O., Alanazi A.M., Hachem K., Suksatan W., Sillanpää M., High-Sensitivity Biosensor Based on Glass Resonance PhC Cavities for Detection of Blood Component and Glucose Concentration in Human Urine, Coatings, 2021, 11:1555 [Crossref], [Google Scholar], [Publisher]
- Mokhayeri Z., Evaluation of the stability of compound 2- fluoro- 1, 3, 2-dioxaphosphinane in axial and equatorial conformations by NBO analysis, Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 2022, 4:104 [Crossref], [Publisher]
- Musa N.M., Sallau M.S., Oyewale A.O., Ali T., Isolation and Characterization of Neoduline from the Rhizome of Dolichos pachyrhizus Harm, Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 2022, 4:113 [Crossref], [Google Scholar], [Publisher]
- Johnson A., Brous A., Samimi A., An Overview of the History of Using Adsorbents in Environment, Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 2022, 4:124 [Crossref], [Google Scholar], [Publisher]
- John B.B., Habila J.D., Oyewale A.O., Tukur A.R., Isolation, Characterization and Antimalarial Evaluation of Methyl-3,12-dihydroxycholan-24-oate from Bovine Bile, Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 2022, 4:135 [Crossref], [Google Scholar], [Publisher]
- Noruzi Moghadam H., Banaei A., Bozorgian A., Biological Adsorption for Removal of Hydrogen Sulfide from Aqueous Solution by Live Eisenia Foetida Worms, Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 2022, 4:144 [Crossref], [Google Scholar], [Publisher]
- Brous A., Johnson A., Samimi A., Investigation of PCM Method for Cathodic Protection of Pipelines, Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 2022, 4:164 [Crossref], [Google Scholar], [Publisher]
- Olaniyi B.O., Oluwaniyi O.O., Oloruntele I.O., Sekoni H.A., Investigation of physicochemical and fatty acid composition of oils from ripe and unripe Blighia sapida fruit, Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 2022, 4:53 [Crossref], [Google Scholar], [Publisher]
- Hosouna B., Malek H.M.A., Abdelsalam S.M.A., Ahwidy Z.D., Computational study of the effectiveness of natural herbal derivatives on COVID-19 virus, Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 2021, 3:323 [Crossref], [Google Scholar], [Publisher]
- Ara I., Maqbool M., Zehravi M., Gani I., Herbs Boosting Immunity in Covid-19: An Overview, Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 2021, 3:289 [Google Scholar], [Publisher]
- Mohammad Asif, Saad Alghamdi, Chemical and Biological potentials of semicarbazide and thiosemicarbazide derivatives and their metals complexes, Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 2021, 3:243 [Crossref], [Google Scholar], [Publisher]


