Document Type : Original Article
Authors
1 Faculty of Dental Medicine, Department of Prosthodontics, Universitas Airlangga, Surabaya, Indonesia
2 dr. Soebandi General Hospital, Jember, Indonesia
Abstract
Rheumatoid arthritis is an autoimmune disease that attacks the joints and causes complaints in the oral cavity, especially periodontitis. This study identified the case of a patient with rheumatoid arthritis, who was missing his teeth and wanted to get dentures made, so he could eat comfortably and restore his aesthetics. Metal framing has been used for a long time because it is lightweight and easy to clean, and does not burden the teeth and periodontal tissues. This article discusses about the use of a partially detached metal framework in rheumatoid arthritis patients. The patient has been receiving therapy for the last three years and continues to do so. There are complaints in the oral cavity in the form of canker sores and shaking, which cause some teeth to fall out. The treatment used in this case was a Removable Denture Prosthesis (RDP) because the patient had many missing teeth and was still under medical care. In this case, a partial RDP with a metal frame is used because it stabilizes the position of the remaining teeth. The results showed that using a removable metal frame satisfies patients partially because it reduces tooth impact and improves aesthetics and chewing ability.
Graphical Abstract
Keywords
Introduction
Rheumatoid arthritis is an autoimmune chronic inflammatory disorder or autoimmune response. People's immune systems can be down and disturbed, destroying joints and lining of the synovial membrane, especially hands, feet, and knees. About 36% of patients reported worsening health and were twice as likely to have their ability to engage in some activities restricted. Furthermore, nearly 30% of patients are more likely to require personal care assistance than persons without arthritis [1]. According to basic health research in 2018, the total of people with rheumatoid arthritis in Indonesia is around 7,30% [2]. Based on the RA prevalence globally (0.5-1%), it is estimated that there are at least 1.3 million people in Indonesia have rheumatoid arthritis [1]. Although there is no permanent treatment for joint inflammation and damage brought on by rheumatoid arthritis, it can be managed with disease-modifying anti-rheumatic drugs (DMARD), corticosteroids, or non-steroidal anti-inflammatory drugs (NSAIDs) [3, 4].
According to Suhaimi et al. [5], rheumatoid arthritis patients were eight times more likely to have periodontal disease. In some studies, rheumatoid arthritis patients experience severe periodontal disease, and tooth loss is more likely experienced by rheumatoid arthritis patients [6, 7]. Periodontitis is a chronic inflammatory condition characterised by degradation of the periodontal ligament and alveolar bone, which can lead to tooth loss if left untreated [8]. According to Potempa et al. [9], periodental disease and rheumatoid arthritis have similar genetic and environmental risk profiles, including high connections with genes associated with immune responses and smoking. They also share aspects of inflammation with nearby bone loss (PD, the bone-supporting teeth; RA, the joint). It has been suggested that one mechanism connecting these two chronic inflammatory disorders is immune responses to infection [10]. Rheumatoid Arthritis Manifestation (RAM) in the oral cavity is marked by stomatitis. Stomatitis happens due to long-term drug use; namely, methotrexate and anti-rheumatic agent. Cyclosporine can cause gingival overgrowth, TMJ disorders, and periodontal disease, including loss of bones and teeth, and xerostomia [11]. The use of partial removable dentures will become the primary method of restoring lost teeth. The proper plan will help preserve the oral cavity, but the worst plan will trigger bone resorption and accelerate the loss of the remaining teeth [12]. Removable partial dentures (RDP) are used in no distal abutment tooth, long span edentulous, and periodontal support conditions in still worse teeth. Bone loss in the visible anterior area with a fixed partial denture will have an unacceptable appearance, physical and emotional problems, primary teeth extraction, patient wishes, and unfavourable maxillomandibular relationships [13, 14]. When a fixed partial denture cannot be used due to the length of edentulous ridge or there is a guarded prognosis for the patient's periodontal condition, RPD is one of the practical solutions used by dentists [15]. Based on the primary material of RDP partial, there are two groups: acrylic resin and metal frame. RDP partial acrylic resin is a denture with acrylic resin bases and a partial metal frame. RDP is a denture whose framework is made of metal. Both materials are available dentures used to replace lost teeth [16]. This study discussed on the denture use in patient with rheumatoid arthritis and periodental disease.
Case report
An older woman aged 62 years old came to the Prosthodontics Clinic, Faculty of Dentistry, Universitas Airlangga, to make maxillary and mandibular dentures so she could eat comfortably and look good. The patient has controlled rheumatoid arthritis and has already been undergoing treatment for three years, and has continued until now. Complaints in the oral cavity were that some teeth had been revoked because of shaking and thrush.
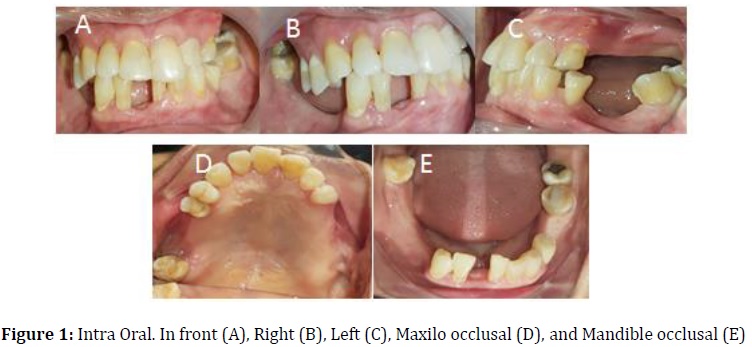
Based on Figure 1 above, the oral hygiene seemed medium and there was a patch on the teeth number 11, 15, 14, 18, 21, 23, 37, 38, and 48; caries on teeth 11 and 21; abfraction on teeth 23 and 34; and lost teeth 16, 17, 24, 25, 26, 27, 28, 35, 36, 41, 44, 45, 46, and 47. On the radiographic examination (Figure 2), there were radiopaque images of dental crowns and root canals 18, impressions of the root canal and dental fillings, radiopaque images of dental crowns on 15, 14, 22, 23, 37, 38, 48, the impression of dental fillings, radiolucent appearance of the crown of teeth 11, 21 impressions of dental caries, missing teeth 17, 16, 24, 25, 26, 27, 28, 36, 35, 44, 45, 46, and 47, and bone loss in region 1, 2, 3, and 4.
When the patient comes to the clinic, informed consent has done. The printing of the study model with printing material irreversible hydrocolloid (alginate) and treatment in the teeth conservation field for teeth 11 and 21 along with providing the education and instruction for treatment of oral cavity health has also done. Then, it is continued in making an individual printing spoon for physiology printing to obtain a job model and bite determination. Preparation was conducted in abutment teeth to make rest seat on teeth 13, 15, 18, 23, 34, 37, and 48. Functional printing of maxillary and mandibular with elastomer medium body is continued with elastomer light body material. Based on those job models, it is made metal frame with Akers clasp design on 15, 18, 34, and 37; RPY clasp on 23, rest addition on 13, c clasp modification on 43, and ring clasp on 48. After the metal frame was finished, a trial fit was carried out (Figure 3), followed by making the bite rim, measuring the vertical dimensions, selecting the color of the teeth, and installing the model on the articulator. The next stage is the arrangement of the maxillary and mandibular teeth and trying them on the patient.


Subsequent laboratory work is making teeth contours acrylic packing, polishing, and inserting dentures on patients. During insertion, pay attention to the retention and stability of denture, esthetics, and patient comfort when using denture, phonetics, occlusion, and patient articulation. The patient was instructed to wear the denture for 24 hours, and the denture should not be used for eating and control the next day. The first and second control a week later, the patient had no complaints, the denture was used to chew food as usual, and the patient was delighted (Figure 4).
Results and Discussion
Fixed Denture Prosthesis (FDP) provides better health and function than Removable Denture Prosthesis (RDP) partial, and most patients prefers using it. However, RDP partial is used in this case because of the lost teeth, a long span edentulous in the posterior part, periodontal support in the worst teeth, the patient still in medical treatment, wishes not to do FDP, which relates to some of the teeth that will be prepared. In addition, it is expensive to make dentures [13]. The treatment with RDP partial will help improve the structure if it can be conducted correctly. RDP partial can be planned to stabilize the teeth' position and to restore arch integrity as a subsequent function unit [12].
Metal frame dentures are ideal than acrylic dentures. Since it is made more thin, rigid, and strong, it can be made an ideal design and more comfortable. In this case, the metal frame can be planned to stabilize the teeth' position in a far away position. Therefore, it can function as a splint in teeth. Because of the patient's systematic condition, using a metal frame is expected not to burden abutment teeth and supporting tissue or alveolar ridge. Hence, it can fulfill a network preservation principle. Besides, the denture is more hygienic [16, 17]. The statement deals with Kazem et al. [18] stated that acrylic removable prosthesis tends to harm periodontium parameters when teeth communicate with resin. However, polyoxymethylene (POM) is advised for those allergic to metal. The simplicity of polymers production using CAD-CAM technology has increased interest in them. Because POM has more muscular flexural strength, microhardness, and fracture toughness than polymethylmethacrylate (PMMA), the denture foundation or framework is designed smaller with less tissue coverage, improving patient oral hygiene and health [15].
Based on the Kennedy classification and survey that have been conducted, edentulous will be affected: retainer types (direct and indirect), connector (major and minor), dentures bases, and RDP partial election [14]. Each component used and designed will control vertical, horizontal, and rotation movement [19]. Retention strength and pressure distribution on the gripping arm are keys to the success of long dentures. In addition, it could be noted that the gripping arm design should only produce a small amount of pressure. This is important so that the remaining tissue is maintained. The lack of stability leads to decreased retention and failure of denture function. The retention strength from Akers gripping is more vital than back action gripping. This research deals with Abdulhadi’s research that the average retention strong is higher than Akers gripping, followed by H-H (half-half) gripping and RPA (rest plate Akers). In this case, Akers claps were used in the teeth 18, 15, 34, and 37 to obtain higher retention strong [19].
RPY (rest, plate proximal, Y-clasp) gripping has a similar mechanism to T-clasp. This design was used in class I or class II Kennedy when the undercut is located near with edentulous area. This clasp lacking is a cast-off accumulation and the condition of flexibility increase from the retention arm, and it could be added bracing and unit stabilization [14]. In this case, RPY was used in the teeth 23 to obtain strong retention. The best addition in the teeth 13 and 23 lacks flexibility from the retention arm. The clinical crown showed a sufficient vertical height when gripping the teeth 43 used to accomodation C-clasp. Meanwhile, ring clasp usage in the teeth 48 is based on the most independent posterior molars, without proximal contact on the mesial side [14]. Besides, the key to success for the RA patient is based on the stability of systemic conditions. During treatment, it could be noted whether there is ulceration, gingival overgrowth, xerostomia, and periodontitis. An imbalance in the oral microbiome might contribute to some oral and systemic disorders. These disorders are head and neck cancer (HNC), periodontitis, dental caries, and recurrent endodontic infections [20]. Meanwhile, antibiotics may help in controlling dysbiosis, and they can further lead to superinfections. After treatment, denture treatment must be delivered, keeping the oral cavity healthy and familiar [11].
Conclusion
This study discusses about a case of using dentures in a patient with a history of rheumatoid arthritis and periodontal disease. The results showed that the patient had lost a lot of teeth, so the used method was a removable denture prothesis with a metal frame. A partially removable metal frame provides satisfaction to the patient because it can reduce tooth shakes and improve aesthetics and chew ability. Moreover, a higher level of oral hygiene is required for RDP patients and that denture design should be as simple as possible. Using metal frame removable dentures on rheumatoid arthritis patients is very effective. Because using a metal frame does not burden abutment teeth and supporting tissue or alveolar ridge, it can fulfil a network preservation principle. Significantly, the gripping design is better planned and applied.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed to data analysis, drafting, and revising of the paper and agreed to be responsible for all the aspects of this work.
Conflict of Interest
We have no conflicts of interest to disclose.
Orcid
Michael Josef Kridanto Kamadjaja
https://orcid.org/0000-0003-3226-7781
Nike Puji Rahmawati
https://orcid.org/0000-0002-4012-4564
Wiwik Herawati Waluyo
https://orcid.org/0000-0002-6446-4264
HOW TO CITE THIS ARTICLE
Michael Josef Kridanto Kamadjaja , Wiwik Herawati Waluyo, Nike Puji Rahmawati. Use of Metal Frame Removable Partial Denture in Rheumatoid Arthritis: A Case Report. J. Med. Chem. Sci., 2023, 6(8) 1878-1884


