Document Type : Original Article
Author
Department of Biochemistry, College of Medicine, Al-iraqia University, Iraq
Abstract
There is a great interest on the role of irisin level in the pathogenesis of many diseases, in particular diabetes mellitus. This research attempted to focus on assessing of irisin levels in type1 diabetes with and without poor glycemic control compared with healthy controls. Irisin is defined as a peptide hormone mainly produced by skeletal muscle. The current study included 40 T1DM patients were subdivided into poor glycemic control (HbA1C>8) and the acceptable glycemic control (HbA1C<8) and 40 healthy control subjects. In the current study, serum irisin was obtained by an enzyme-linked immune sorbent assay (ELISA). Likewise, the additional parameters such as FBG, HbA1c, and lipid profile were measured by a spectrophotometer. The results expressed that the serum level FBG, HbA1c, TC, TG, LDL, and VLDL were elevated significantly in T1DM patients with poor glycemic control compared with control group, and also to the other patients groups (p<0.001). Moreover, Serum irisin level was negatively associated with HbA1c. Finally, the irisin level was lower in T1DM with all stages of glycemic control particular with poor glycemic group.
Graphical Abstract
Keywords
Main Subjects
Introduction
T1DM alters many elements of macro-nutrient metabolism, although the main disease characters represented in carbohydrate metabolism alteration [1, 2]. Because pancreas cells are destroyed by the immune system and require the exogenous insulin to survive, T1DM is linked to inadequate insulin secretion [3, 4].
Irisin was initially identified in 2012 as an exercise-induced hormone excreted through the skeletal muscle. About (112) amino acids forms the structure of Irisin and it promotes the formation of the brown-adipocyte-like cells in mice [5].
The origin of irisin term comes from the Greek Goddess "Iris" who represented the messenger among the Gods. The skeletal muscle has been represented as an organ that secretes substances and can communicate with other tissues and organs. It has to contract to produce numerous proteins. Consequently, being inactive may result in impaired muscular responsiveness [6].
Irisin and myonectin are important myokines secreted in response to the physical exercise promoting the dietary glucose and fatty acids uptake that oxidized in liver and adipose tissue [7].
It can be created in the skeletal muscle and heart, and also has an essential role in the conversion process of white adipose tissue to the brown adipose tissue [8], enhancing glucose uptake in skeletal muscle and heart via calcium/ROS and P38 AMPK mediated the AMPK pathway, improving hepatic glucose and lipid metabolism, and promoting pancreatic β cell function [9, 10]. The research attempted to focus on the role of irisin level in the pathogenesis of type1 diabetes.
Materials and Methods
Subjects
The following research includes 40 patients with T1DM involves (20 females and 20 males) and 40 control subjects matched in age and gender and their ages ranged from 15-38 years old. The controls were selected as clear from acute and chronic diseases. Patients were selected from Baghdad Teaching Hospital, Medical City Baghdad, Iraq. The study involved most anthropometric measurements such as BMI, the height, the weight, the age, and sex. The exclusion criteria for this study were type2 diabetes and the pregnant women.
Two methods were utilized:
- Irisin was quantified following Enzyme-linked immunosorbent assay (ELISA) by using (Bio-source/USA) kit.
- Lipid profile, FPG, and HbA1c were quantified following enzymatic colorimetric methods by spectrophotometer through human Gesellschaft four biochemical and mbHMax-PlanckGermany kits.
Statistical analysis
The research used the Statistical Package (SPSS-23). The data presented as means ± SD. (ANOVA test) was be used to show the difference between groups. (T-test) was used to show the difference between pair of groups. Likewise, Pearson correlation summed the correlation between variables. The significance was acceptable at 0.05 and 0.01.
Results and Discussion
After HbA1c measurement, the total number of patients was 40 participants were divided into two groups according to the glycemic control groups (poor and acceptable) and each group involved 20 participants. Table 1 indicates that Glycated hemoglobin was found to be higher in diabetic patients compared with the control subjects and significantly increased in poorly control patients than the acceptable control patients and healthy subjects (P 0.05).
Table 2 presents the bibliography of research data and evolution of the mean difference of parameters measured in the studied groups.
Serum irisin level
The mean levels of serum irisin for patients group (poor and acceptable) were (14.04±0.79 and 15.01±0.55 ng/ml), respectively, and in the control healthy group was (20.19±2.03 ng/mL).
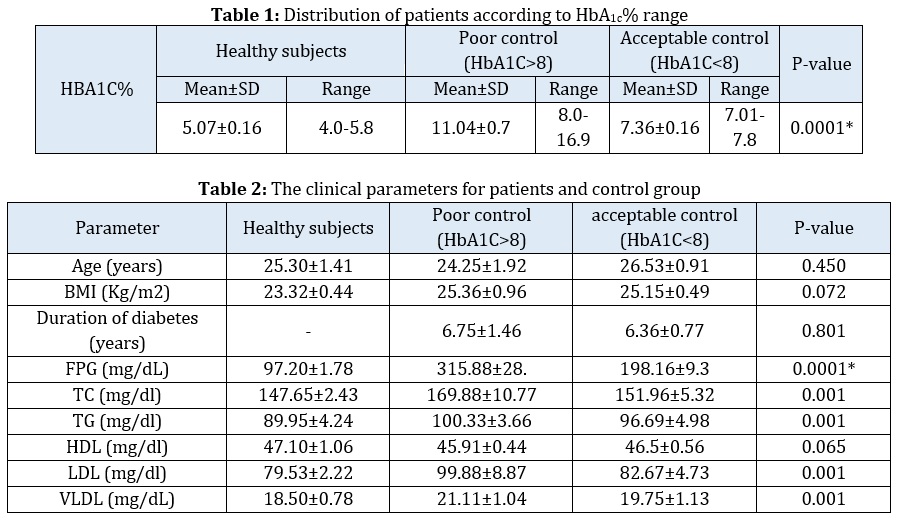
Figure 1 and Table 3 demonstrate the decreased irisin level for patients groups as comparing that in healthy group and in particular poor control patients recorded the lower levels, and a significant decrease mean of irisin (p<0.001 and p<0.005, respectively). Whereas, no significant difference of irisin level was found between the acceptable and poor groups, as demonstrated in Table 3.
Correlation of serum irisin with other parameters under study
Table 4 indicates the correlations of irisin with corresponding parameters in the current research. To investigate the irisin impact on the investigated parameter (The r-value of correlation was not significant between irisin and age, BMI, duration, TC, TG, HDL, LDL, and VLDL. In contrast, it a significant negative correlation of irisin was found with glucose and HbA1c in the poor glycemic control patient group.
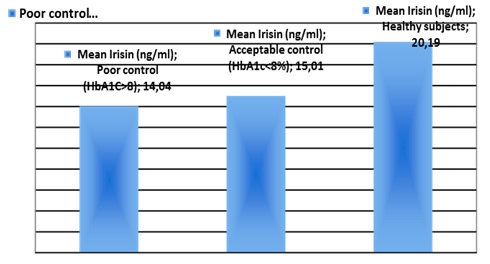
Figure 1: The mean irisin in studies group


This study reflects the irisin role in T1DM to evaluate the impact of irisin on the mean of glycemic control, particularly the hyperglycemic effect on stimulating the complications growth in diabetes. The present data noted T1DM patients and controls shared them that both subjects showed a gradual decreased mean of irisin. Besides, the relation has been examined between decrease in irisin level and reduced glycemic control. The main findings of our study were that poor glycemic control patient of irisin level were lower than the other patients and the healthy subjects. This indicates that the irisin level is strongly affected by glycemic state. Thus, irisin has an evidently important role in inflammatory reactions and wound healing [11].
A number of mechanisms have been projected for this issue. Irisin has an extent effect on protecting the function of endothelial cell, besides minimizing the endothelial damage. Likewise, the lower irisin level is accompanied with atherosclerosis and a high degree of the advanced glycation end product and inflammation [12].
Such a finding is in agreement with other investigators who demonstrated a similar link [13]. In addition, the study has been noted that hyperglycemia was associated with the decreased irisin levels. They have revealed the decreased irisin level when hyperglycemic existed. To sum up, these findings may suggest that irisin could have the most important impact on monitoring DM.
Besides, the finding of the current study resembles those found by (MF Faienza) who reported that in better glycemic control of type 1 diabetic patients, serum Irisin was significantly increased [14]. Likewise, Deng reported that serum Irisin level was significantly lower in patients with CAD as compared with the healthy controls [15]. The current results are not consistent with other studies where serum irisin was found to be increased in T1DM [16].
The results of the current study are in agreement with researcher who reported a negative correlation with HbA1c and OGTT; meanwhile, these results were inconsistent with others who reported a positive correlation for serum Irisin with FPG and HbA1c [17, 18].
A recent study was done to elucidate the vital role of Irisin in the pathophysiology of T2DM in which Irisin stimulates glucose uptake in the skeletal muscle and improves lipid and the glucose metabolism of the liver, and thus improving hyperglycemia, hyperlipidemia, and IR [19].
In addition, others reported that Irisin is considered as a cellular ‘energy sensor‘. The low level of Irisin blocking the conversion of white adipose tissue to the brown adipose tissue, resulting in decreased metabolic thermogenesis [20].
Generally, the liver and the lymphoid organs are the major sites of inflammatory mediator production. However, the investigations have shown that white adipose tissue (WAT) also expresses many pro-inflammatory and anti-inflammatory factors and in this respect, it probably contributes to the increase of circulating levels of the inflammatory markers in diabetes.
Accordingly, the lower expression of irisin reflects glycemic complication and the irisin level may have the therapeutic effects in diabetes.
Conclusion
Irisin is inversely affected as diabetes persists with or without the glycemic control, also decreasing the irisin level is significantly related to hyperglycemia. Thus, Irisin level may suggest to be affected by inflammation, autoimmunity, and the T1DM severity.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed to data analysis, drafting, and revising of the paper and agreed to be responsible for all the aspects of this work.
Conflict of Interest
The author declared that they have no conflict of interest.
ORCID:
Najlaa Abed Jassim
https://orcid.org/0000-0002-9407-4996
HOW TO CITE THIS ARTICLE
Najlaa Abed Jassim. Estimation of Irisin and Some Biochemical Parameters in Diabetes Mellitus Iraqi Patients. J. Med. Chem. Sci., 2023, 6(4) 809-815
https://doi.org/10.26655/JMCHEMSCI.2023.4.12
URL: http://www.jmchemsci.com/article_158662.html


