Document Type : Original Article
Authors
1 Chemistry Department, College of Science, Al-Muthanna University, Iraq
2 College of medicine, Al Muthanna University, Iraq
Abstract
Mortality of coronavirus disease (COVID-19) was elevated all over the world since 2019 due to its mainly spread through the respiratory route and mass contact. Many risk profiles on coronavirus illness progression has been previously studied. This study aimed to describe several factors associated complications, gender, age, D-dimer, and risk profile of mortality with COVID-19. This study summarizes the hematological characteristics and laboratory markers of COVID-19 non-survivors and those who continue to live after healing from COVID-19 in AL-Muthanna governorate, a small town in the south of Iraq.
Graphical Abstract
Keywords
Main Subjects
Introduction
Coronavirus pathogen (COVID-19) is a disease firstly identified in Wuhan, China on December 31, 2019 has caused great complications to human health all over the world. Generally, this virus was transmitted and rapidly spread from person to another especially by exhaling respiratory droplets and smaller aerosol particles containing his virus [1]. A large population of patients infected with (COVID-19) disease showed many clinical signs, involving mild breathing issues and recover with hospitalization to moderate illness and multiple organ dysfunctions [2]. However, some patients improve seriously complications, destroy lung tissue resulted pneumonia, and eventually die of the illness at any age [3]. With the first symptoms of the disease, more mortality cases have been reported with the older people or patients have specific comorbidities, such as diabetes, cardiovascular, cancer, or severe acute respiratory disease [4]. Diagnosis and monitoring of earlier complications can allow doctors offer protection, keep patients lifesaving, and control mortality [5]. Biochemical laboratory tests such as complete blood count CBC and D-dimer status, Cytokine tests, C-reactive protein (CRP) are essential for assessing and detecting disease progression [6]. Another study focused on determining high blood sugar, liver function tests as factors to increase chances of death in more COVID-19 patients [7]. In this current study, the hematological markers and liver function tests were explored and estimated for 290 COVID-19 patients (survivors and died) in AL-Muthanna governorate from February 2020 to January 2021.
Materials and Methods
Data collection
This study was conducted at AL-Hussein Teaching Hospital in AL-Samawa Province as in Figure 1. Patients with biochemistry data were involved in the study if they were hospitalized in the intensive healthcare units between February 2020 and January 2021. All (n=260) are affected and diagnosed as COVID-19 patients with severe symptoms. Cases are divided into two groups (survivals and death). The data available included the following biochemical tests were examined for all patients: liver tests profile, kidney function profile, hematological and coagulation profile, CRP, ferritin, sodium, potassium, and troponin. Furthermore, to assess the factors affected death of patients with COVID-19, gender, age, and sex in addition to clinical characteristics have been examined such as diabetes mellitus, hypertension, and CVD. All Patients were treated clinically according to the universal COVID-19 management guidelines.

Figure 1: Location of the study area
Statistical analysis
All study tests were performed and expressed as (mean ± SD) standard deviation, p-value (p<0.05) was considered as statistically significant. All statistical values were analyzed by using SPSS software (Version 18).
Results and Discussion
A total of adults patients (N=260) with age (40-60 years old). Sixty-five hospitalized patients were died with a median age of 50 years old, which was higher compared with the survivors group. The older ages had shown a higher number in death than the youngest of the rest of infections cases. The general characteristics data were illustrated in Table 1. Complete blood count cells indicated that immune system cells (neutrophil) number were greatly higher in the death group, as compared with survivors. In addition, the lymphocyte count in survivors recorded increased in number, as compared with death. In terms of hemoglobin levels (Hb), the survivors indicated a higher Hb level than the death. Moreover, there was also an increase in the D-dimer level among the groups (P > 0.05) (Tables 2 and 3).
The estimation of hepatic tests revealed that ALT, AST, and total bilirubin were increased highly in all patients. The death showed high abnormality levels of these enzymes compared with survivors. Furthermore, the patients showed a high D-dimer and CRP. Concerning the results of kidney tests, there were no great changes in urea, creatinine between death and survivors.
The importance of biochemical markers in diagnosis COVID-19 still needs more clinical efforts to provide clear information for prognostication of this disease. However, there are lots still under investigation about COVID-19 effects on variable biochemical and hematological tests in infections who survived or died due to risk factors for COVID-19 mortality. The study revealed that the median age of infectious who not-survived was higher than survived (Table 1).
The older patients have the hazard and susceptible to death than the younger and this may be the reason of high population of death among the elder COVID-19 patients. Our results are matched with [8] who reported that ageing influences T-cells and B-cells functions. Males are higher hospitalized coronavirus and mortality than females. Our results confirmed that diabetic, hypertension, and CVD are more associated with contribution with COVID-19 mortality. As indicated in Tables 2 and 3, coagulation factors performed within the first day admission to hospital tended to record elevated levels in non-survivors compared with survived patients. Hence, the infections treatment should considered the high risk factors related the clinical coagulation parameters, Prothrombin time (PT) and D-dimer are significant parameter for identifying prognosis and severity of COVID-19 which recorded a higher number in death than alive infections [9]. Similar to PT and D-dimer, the available data in this study showed higher neutrophil in non-survivors than survivors, while lymphocytes recorded no differences between the death and who lived.
Table 1: Demographic characteristics

Table 2: Clinical characteristics of non-survivors patients with COVID-19 (N = 195)

Table 3: Clinical characteristics of survivors patients with COVID-19 (N = 65)
|
Clinical characteristics |
Normal value |
Mean ± SD |
|
White blood cell count × 109/L |
3.5-4.5 |
6.9 ± 1.3 |
|
Neutrophils count × 109/L |
1.8-6.3 |
55.09 ± 11.14 |
|
Lymphocytes count × 109/L |
1.1-3.2 |
1.0 ± 1.07 |
|
Platelet × 109/L |
125-350 |
199.29 ± 2.44 |
|
Hb, g/L |
11.5-15.0 |
11.40 ± 1.11 |
|
PT, s |
9-14 |
12.56 ± 3.40 |
|
PTT, s |
20-40 |
32.14 ± 10.01 |
|
Na, mmol/L |
135-145 |
130.29 ± 1.57 |
|
K, mmol/ L |
3.5-4.5 |
3.75 ± 0.34 |
|
Cl, mmol/L |
95-105 |
97.77 ± 11.15 |
|
AST, U/L |
8-40 |
66.24 ± 75.32 |
|
ALT, U/L |
5-35 |
60.53 ± 1.19 |
|
LDH, U/L |
109-245 |
201.20 ± 111.44 |
|
Direct bilirubin, mmol/L |
0.1-0.3 |
0.55 ± 1.10 |
|
Indirect bilirubin, mmol/ L |
0.2-0.8 |
0.91 ± 1.09 |
|
TBIL, mmol/L |
3.4-20.5 |
1.29 ± 2.63 |
|
CRP, mg/L |
0-10 |
30.73 ± 29.67 |
|
D-dimer, ng/mL |
<250 |
423.69 ± 202.43 |
|
PaO2, mmHg |
75-100 |
90.25 ± 11.2 |
|
Albumin g/dL |
3.4-5.4 |
3.6 ± 2.01 |
|
Ferritin ng/ml |
20-435 |
155.67 ± 8.11 |
|
Troponin ng/mL |
0.1-0.3 |
0.5 ± 0.01 |
|
Urea mg/dL |
15-40 |
50.3 ± 43.3 |
|
Creatinine mg/dL |
0.5-1.2 |
0.9 ± 0.3 |
Neutrophilia was considered as an indicator of the cytokine storm and inflammatory syndrome which usually occur as a genetics pathogen factor in COVID-19 and associated diseases [10-12]. However, many studies suggested Neutrophilia with a high number might also result due to the bacterial infection [13]. In terms of C-reactive protein (CRP) which formed by liver, various inflammatory states were greatly increased. Our analysis showed the significant elevated levels of D-dimer in non-survivors group, as compared with survivor group. These findings are in agreement with [14] who observed that CRP elevated in 75-93% COVID-19 infections, especially in mild and severe disease. Liver enzymes like other biochemical parameters, increased levels of these biochemical markers were recorded in non-survivors people associated with more sever disease in COVID-19 patients, as compared with survivors group [15-17]. The abnormalities in these liver parameters demonstrate that COVID-19 virus when effected human may cause hepatocytotoxicity, heart injury, and other human organs. Our results are in agreement with [18, 19]. The results indicated no notable changes related to the level of serum bilirubin considered as an indicator in many dysfunctions in biliary diseases. These finding are similar to [20]. Besides, our results respect to serum creatinine which synthesized as a product of protein breakdown in the liver and excreted by the kidney, observed no significant change between the death and survivors. The results revealed no association related to kidney tests with COVID-19 death. Our observations are consistent with a recent study that showed the high levels of creatinine in COVID-19 patients with severe disease [21].
Conclusion
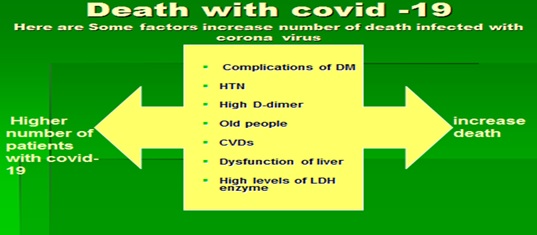
This study showed a significant influence of complications and demographic factors involving diabetes (DM), HTN, CVDs, high levels of D-dimer, and older males with comorbidities on COVID-19 mortality. These results might facilitate the disease’s future diagnosis, control, prevent, and treatment. In this study, liver function tests were intensively related to COVID-19 mortality. Non-survivors showed higher levels of TBIL, AST, ALT, and lactate dehydrogenase enzyme. Assessment of these liver clinical tests might help clinicians to control and assess the COVID-19 prognosis.
Acknowledgments
The authors would like to acknowledge Dr. Kasim M. Hello, Muthana university for his proof reading.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed to data analysis, drafting, and revising of the paper and agreed to be responsible for all the aspects of this work.
Conflict of Interest
There are no conflicts of interest in this study.
Orcid:
Muna Hasson Saoudi
https://orcid.org/0000-0002-0771-962X
Ihab Abbas Taher
https://orcid.org/0000-0002-1501-7652
HOW TO CITE THIS ARTICLE
Muna Hasson Saoudi, Ihab Abbas Taher. Hematological Profile and Liver Biomarkers of COVID-19 Non Survivors in Iraq. J. Med. Chem. Sci., 2022, 5(7) 1357-1363