Document Type : Original Article
Authors
1 Department of Thoracic Surgery, Hazrate Rasoul Akram Hospital, Iran University of Medical Science, Tehran, Iran
2 Research Fellow, Rockingham Medical Research Center, ADKWA Medical, Perth, WA, Australia
3 Research Committee Member, Faculty of Medicine, Iran University of Medical Science, Tehran, Iran
Abstract
In a retrospective multi-center study from August 2019 to Dec 2020, patients with chest trauma and stable hemodynamics who underwent VATS within their first week from traumawere enrolled in hospital. The electronic recordswere collected and reported on demographics, surgical procedure details and postoperative complications. In a sample of 44 participants, the mean age was 31.21±9.21 and 39 participants were male (88.6%). Sixteen people had blunt trauma, and 28 people had penetrating trauma. Accompanying organ damage was reported in 9 patients (20.5%). The mean injury severity score was 20.98±6.74. In the sample, the duration of surgery was 70.52±21.02 minutes, the number of days with a chest tube was 5.95±4.40, duration of ICU staywas 7.77±4.30 days, duration of hospitalizationwas12.36±1.98 days andduration of return to physical activity was 7.56±1.48 days. Among patients, one patient (2.3%) was intubated. Postoperative imaging findings were positive in 11 patients (25%). During postoperative hospitalization, the most common findings were surgical site infection in 4 (9.1%) empyema in 3 (6.8%), pneumothorax in 3 (6.8%), pneumonia in 2 (4.5%), hemothorax in 2 patients (4.5%) and death in 1 (2.2%).VATS is associated with lower complications, as well as higher patient tolerance than other methods; Making it a safe and effective method of controlling acute chest trauma in patients with hemodynamic stability in young adults.
Graphical Abstract
Keywords
Main Subjects
Introduction
Chest trauma is considered a leading cause of death up to 25% of all traumatic mortality in urban centers [1,2]. Previously open thoracotomy and tube thoracostomy as two major surgical procedureswere the treatment of choice for investigative and curative operations in chest trauma, yielding a notable 5 to 80% rate of postoperative complications [3]. The development of video-assisted thoracoscopic surgery (VATS) in the last decade has turned it into a new option for the management of chest trauma in patients with stable hemodynamics (Figure 1) [4,5].

Figure 1: Safety and complications of medical thoracoscopy in the management of pleural diseases
Regarding the high ratio of chest trauma patients with stable hemodynamics and no contraindications, the VATS can be considered as the treatment of choice on a majority of the patients to decrease the risk of operation and postoperative complications [6]. Several studies showed positive results with VATS for chest trauma injuries, including retained hemothorax [7] and also safety and efficacy of the procedure [8,9].
It is estimated that up to 85% of all chest traumatic patients can be managed initially with thoracostomy tube and hemodynamic support; of these, 20-30% will need further intervention due to continued bleeding, retained hemothorax and pneumothorax [10,11]. These patients benefit the most from VATS surgery. Compared to other methods, VATS lower postoperative pain complaints, better aesthetic outcome, a full optical view of intrathoracic organs and also prevents the need for major surgeries and their complications [8,12]. Although several studies have been conducted, there are few to evaluate the efficacy, morbidity and mortality of early VATS (rather than late surgery) for the management of chest trauma in patients.
In the current study, we aim to evaluate the chest trauma patients with stable hemodynamics, who primarily underwent video thoracoscopic surgery in the first week after trauma, to achieve a comprehensive view on surgical details, perioperative and postoperative complications.

Figure 2: Augmented reality and 3-dimensional printing Technologies for guiding complex thoracoscopic
Material and Methods
Study design and participants
The present study is a cross-sectional, observational, multi-center study conducted between August 2019 and December 2020 at two tertiary medical centersin Rasul Akram and Haftom e Tire hospitals, Tehran, Iran. The study protocols were designed according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement and approved by the Iran University of Medical Sciences ethics committee.
We recruited a consecutive census of all patients with chest trauma and stable hemodynamics who underwent only VATS within the first week after surgery. The patients who died at their arrival, those who underwent emergent thoracotomy orany other surgery, those who were discharged without intervention, and patients more than seven days from initial trauma were excluded. Using electronic records, patient’s demographics and clinical information's including age, gender, type of trauma, mechanism of trauma, injury severity, hospitalization period(days), ICU stay period (days), number of days with a chest tube, need for intubation, days under assisted ventilation was were recorded. The injury severity was measured at their initial arrival using injury severity score (ISS) ranging from 1 to 75 for all patients [13]. The postoperative variables: occurrence of hemothorax, pneumothorax, empyema, pneumonia, surgical site infection, need for painkillers, and days to return to normal activity level were also collected for patients.
Bias
The risk of bias for the clinical judgment was minimized by associating the clinician's judgment directly to the ISS scoring system. All initial assessments were done by medical interns, surgery residents and their supervising professor at the time (Figure 3).

Figure 3: Examples and observations of a confirmation bias
Statistical Analysis
Continuous variables were presented as mean ± standard deviation (SD), and categorical variables were described in frequency and percentage. Preliminary analyses showed no outliers. The data was reported in the forms of text, tables and figures. The statistical analysis was performed using SPSS version 23 (Figure 4) (SPSS Inc. Chicago, I).

Figure 4: Statistical analysis - complex systems and AI
Results and Discussion
Patients Characteristics and Clinical Data
Forty-four patientswere enrolled in the study. The mean age was 31.23±9.21, the participants were mostly male (88.6%). Of 44 patients, 16(87.5) had blunt, and 28(63.6) had a penetrating injury. The multiple organ injury was observed in 35(79.5), and the mean ISS was 20.98±6.74. The patient characteristics and clinical data are summarized in Table 1.

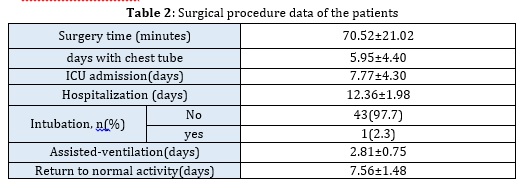
Surgical Procedure Data
As seen in Table 2, the mean surgery time was 70.52±21.02 min. The patients’ average number of days with a chest tube, hospitalization, ICU admission, assistedventilation and return to normal activity were 5.95±4.40, 12.36±1.98, 7.77±4.30, 2.81±0.75 and 7.56±1.48 days, respectively. Only one patient (2.3%) was intubated during their post-surgery hospitalization.
Postoperative Complications
During the time from surgery to discharge, imaging findings were positive in 11 patients (25%). The most common findings were surgical site infection in 4 (9.1%) empyema in 3 (6.8%), pneumothorax in 3 (6.8%), pneumonia in 2 (4.5%), hemothorax in 2 patients (4.5%) and death in 1 (2.2%). Figure 1 reveals the complications in the form of bars and counts (Figure 5).
This study investigated the postoperative complications of early VATS surgery in chest trauma patients. 25% of patients had postoperative radiologic findings. The most common postoperative findings were surgical site infection, empyema and pneumothorax. There was only one death among 44 patients during their hospitalization.
Previously open surgery was considered as the treatment of choice in the management of chest trauma injuries. Thoracotomy complications rise up to 80% [3] with a longer period of recovery, even in limited injuries [14, 15]. The postoperative complications of open surgery cause a load of physical discomfort for the patients. The prevalence of post-surgical pain syndrome is estimated at 25% in this type of surgery [16]. In the last decade development of VATS turned it into a favorable choice for the management of chest trauma injuries in patients with stable hemodynamics. And several studies have gone through its safety, efficacy and feasibility. VATS is known as a procedure with low risks and high efficacy for retained hemothorax and pneumothorax, empyema, observation of diaphragm and mediastinum [9].
The postoperative pain, air-leak, hospitalization and life quality improve after VATS compared to other methods [19, 24]. Our results showed that these complications are also similarly favorable in patients with recent chest trauma.
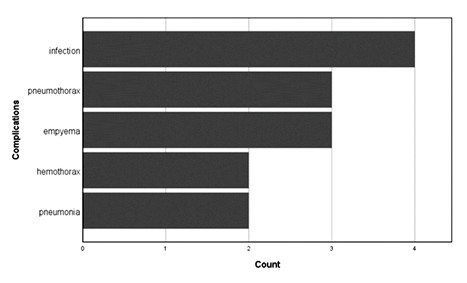
Figure 1: Postoperative complications of the patients (one patient was dead and excluded from this figure)
In a similar study on 37 patients with similar age men, the most patients were male. The higher prevalence of male individuals (95%) in that study and in our study (88%) is attributable to higher rates of violence and MVCs among young male adults [12]. The exact time of VATS is controversial in the literature. We enrolled the patients with first-week VATS. Similarly, Landreau et al. and Heniford et al. suggested the surgery at the earliest time, particularly the first seven days after trauma[17, 18]. Regarding retained hemothorax, Meyer et al. demonstrated that the VATS within the first three days after trauma yields a lower rate of hospital stay and complications [19]. On the other hand, recent investigations by the American traumatic surgery association showed no association between the time of surgery and the success in hemothorax resolution [20-22].
Studies showed that elderly adults have a higher chance of changing plans from VATS to open surgery since the hemodynamic stability is harder to maintain [23-25]. Hemodynamic stability is a prerequisite for VATS surgery.
The total surgery time in VATS is similar to open thoracotomy. In a Comparison, Goodman et al. [16] showed that VATS and open thoracotomy have 72 and 68 min lengths on average. Moreover, our results implied the need for painkillers in 38% of patients compared to 45% in that study. Such complications like the pain are associated with the higher experience of the surgery team [25]. Moreover, the number of days with a chest tube in VATS is significantly lower than open surgery [26].
Conclusions
Post-traumatic infections after trauma are one of the most important causes of elongation of hospital stay and take a lot of effort from physicians to overcome. The VATS can serve as an effective way for drainage of infectious collections since it gives a better view than other methods such as tube thoracotomy. The hospitalization period in VATS and return to normal activity is shorter than open surgery due to less invasive procedure. It was reported that, since 50% of patients with suspected diaphragmatic injury have negative findings on open surgery, they might highly benefit from a lower risk of mortality in VATS. In conclusion, early VATS is a reliable, safe, and efficient method to manage chest trauma. This surgery has a low rate of complications and better compliance for the patients. The low rate of mortality and morbidity turned it into a good choice for the treatment of chest trauma in patients with stable hemodynamics.
Acknowledgments
We would like to show our gratitude to the Rasool Akram Medical Complex Clinical Research Development Center (RCRDC) for its technical and editorial assists.
Financial Support:
This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors. The content is solely the responsibility of the authors.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Authors' contributions
Study concept and design: SMHK
Acquisition of data: MK, FJ
Drafting of the manuscript: MK, AT, FJ
Critical revision of the manuscript for important intellectual content: All the authors
Study supervision: SMHK
Literature searching: FJ, MK
All authors read and approved the final manuscript.
Ethical Approval
Not applicable.
Conflict of Interest
There is no conflict of interest to declare.
ORCID
Amirhossein Tafreshian:
https://www.orcid.org/0000-0002-2630-9335
Seyed Masoud Haghighi Kian:
https://www.orcid.org/0000-0003-3533-8055
HOW TO CITE THIS ARTICLE
Mehdi Khosravi, Fatemeh Jahanshahi, Amirhossein Tafreshian, Seyed Masoud Haghighi Kian. Medical Evaluation of Mortality and Complications of Thoracoscopic Surgery with the Help of Primary Video in Patients with Thoracic Trauma with Stable Hemodynamics, 2019-2020, J. Med. Chem. Sci., 2022, 5(3) 361-368
DOI: 10.26655/JMCHEMSCI.2022.3.10
- Aseni P., Rizzetto F., Grande A.M., Bini R., Sammartano F., Vezzulli F, Vertemati, M., J. Surg., 2020, 221:1082 [Crossref], [Google Scholar], [Publisher]
- Fard A.M.M., Fard M.M., Eurasian J. Sci. Tech., 2021, 1:284 [Crossref], [Google Scholar], [Publisher]
- Jones K.W., Clin. North Am., 1980, 60:957 [Crossref], [Google Scholar], [Publisher]
- Fisher B.W., Majumdar S.R., McAlister F.A., J. Med., 2002, 112:219 [Crossref], [Google Scholar], [Publisher]
- Abolhoda A., Livingston D., Donahoo J., Allen K., J. Cardiothorac. Surg., 1997, 12:356 [Crossref], [Google Scholar], [Publisher]
- Carrillo E.H., Kozloff M., Saridakis A., Bragg S., Levy J., Trauma Acute Care Surg., 2006, 60:111 [Crossref], [Google Scholar], [Publisher]
- Bagheri R., Tavassoli A., Sadrizadeh A., Mashhadi M.R., Shahri F., Shojaeian R., Cardiovasc. Thorac. Surg., 2009, 9:195 [Crossref], [Google Scholar], [Publisher]
- Navsaria P.H., Vogel R.J., Nicol A.J., Thorac. Surg., 2004, 78:282 [Crossref], [Google Scholar], [Publisher]
- Manlulu A.V., Lee T.W., Thung K.H., Wong R., Yim A.P., J. Cardiothorac. Surg., 2004, 25:1048 [Crossref], [Google Scholar], [Publisher]
- Ahmed N., Jones D., Injury, 2004, 35:479 [Crossref], [Google Scholar], [Publisher]
- Lang-Lazdunski L., Mouroux J., Pons F., Grosdidier G., Martinod E., Elkaı̈m D., Azorin J., Jancovici R., Thorac. Surg., 1997, 63:327 [Crossref], [Google Scholar], [Publisher]
- Motaharian E.S., Mahmoodiyeh B., Lorestani S., Sadri M.S., Fard M.M., Fard A.M.M., Amini A., Chem. Rev., 2021, 3:171 [Crossref], [Google Scholar], [Publisher]
- Mokhtare M., Alimoradzadeh R., Agah S., Mirmiranpour H., Khodabandehloo N., Middle East J. Dig. Dis., 2017, 9:228 [Google Scholar], [Publisher]
- Etemadi S., Mahmoodiyeh B., Rajabi S., Kamali A., Milanifard M., Romanian Soc. Cell Biol., 2021, 25:2417 [Google Scholar], [Publisher]
- Carrillo E.H., Heniford B.T., Etoch S.W., Polk H., Miller D.L., Am. Coll. Surg., 1997, 184:316 [Google Scholar], [Publisher]
- Ben-Nun A., Orlovsky M., Best L.A., Thorac. Surg., 2007, 83:383 [Crossref], [Google Scholar], [Publisher]
- Rutledge R., Osler T., Emery S., Kromhout-Schiro S., Trauma Acute Care Surg., 1998, 44:41 [Crossref], [Google Scholar], [Publisher]
- Sihoe A.D., Lee T.W., Wan I.Y., Thung K.H., Yim A.P., J. Cardiothorac. Surg., 2006, 29:795 [Crossref], [Google Scholar], [Publisher]
- Knoll H., Ziegeler S., Schreiber J.U., Buchinger H., Bialas P., Semyonov K., Graeter T., Mencke T., Anesthesiology, 2006, 105:471 [Crossref], [Google Scholar], [Publisher]
- Goodman M., Lewis J., Guitron J., Reed M., Pritts T., Starnes S., Emerg. Trauma Shock, 2013, 6:106 [Crossref], [Google Scholar], [Publisher]
- Landreneau R.J., Keenan R.J., Hazelrigg S.R., Mack M.J., Naunheim K.S., , 1996, 109:18 [Crossref], [Google Scholar], [Publisher]
- Heniford B.T., Carrillo E.H., Spain D.A., Sosa J.L., Fulton R.L., Richardson J.D., Thorac. Surg., 1997, 63:940 [Crossref], [Google Scholar], [Publisher]
- Meyer D.M., Jessen M.E., Wait M.A., Estrera A.S., Thorac. Surg., 1997, 64:1396 [Crossref], [Google Scholar], [Publisher]
- Bahadori F., Sahebazzamani Z., Zarei L., Valizadeh N., Tehran Univ. Med. J., 2018, 76:608. [Google Scholar], [Publisher]
- Mattox K.L., Wall Jr M.J., Chest Surg. Clin. N. Am., 2000, 10:167x [Google Scholar], [Publisher]
- Liu D.W., Liu H.P., Lin P.J., Chang C.H., Trauma., 1997, 42:670 [Crossref], [Google Scholar], [Publisher]


